Figure 2: Graphical representation of the respiratory and circulatory systems.
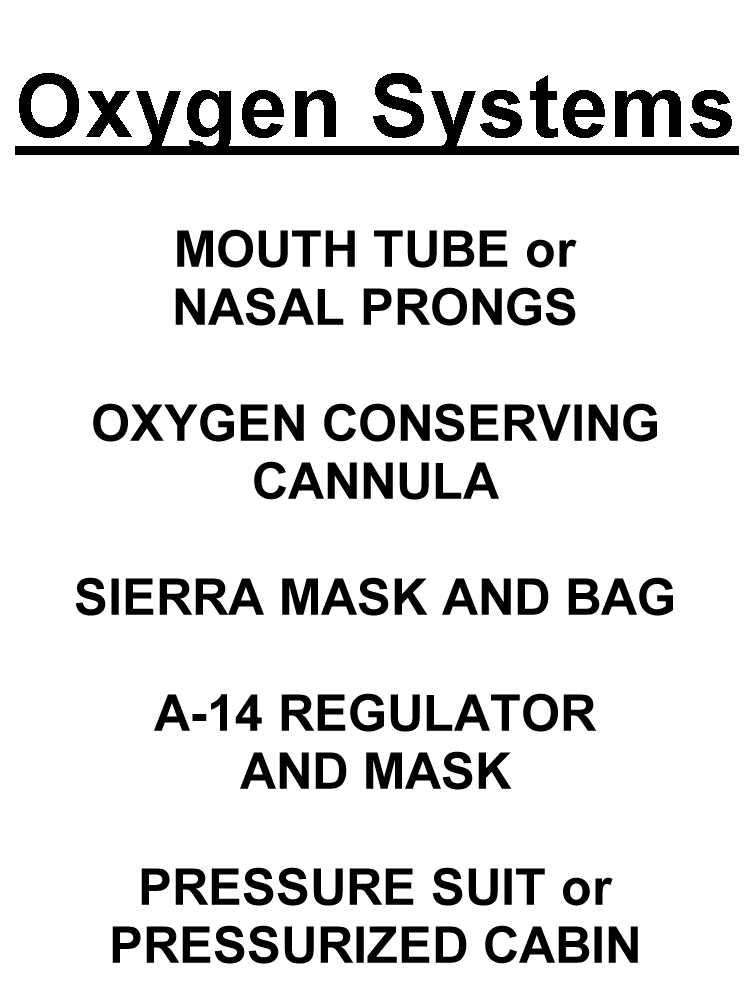
Types of oxygen delivery systems
Mouth tube or nasal prongs
Oxygen conserving canula
Sierra mask and reservoir bag
A-14 regulator and mask (100% and pressure breathing)
Pressure suit or pressurized cabin
Thu Jan 25 19:04:32 2001
From: Steele Lipe <slipe@earthlink.net>
Copyright 1995 Steele Lipe MD
Revised 2002, Daniel L. Johnson MD
Note: figure numbers in this draft correspond to the current file names, and begin with #2.
OXYGEN TALK
Given at the SSA CONVENTION
RENO, NV.
4 MARCH 1995,
Steele Lipe
2539 Ardath Rd.
La Jolla, CA 92037-3502
(858)456-7242
(858)456-2764 fax
slipe@earthlink.net
Without oxygen we couldn't exist. As soaring pilots we wish to fly high; but since the amount of oxygen in the atmosphere decreases with altitude, some pilots have ended their existence by flying high.
Our understanding of oxygen and its use at altitude is based soundly on physiologic principles: we stay alive by observing these principles and respecting the limits of our selves and our equipment.
Why do we need oxygen? All our cells use oxygen to extract energy from food; without oxygen our muscles are weak -- and also our brains!
The reason that we need to write articles about oxygen is that our bodies do not have a oxygen-level detector. Low oxygen does not cause shortness of breath, or air hunger, or anything of the sort. Even with severe oxygen lack, we feel good, we feel confident, we feel happy, even while we run low on oxygen and are making stupid decisions. Yet making decisions is what soaring is all about:
Wise decisions come from good judgment.
Good judgment comes from experience.
Experience comes from poor judgment.
...Experience is something you get shortly after you need it.
Respiration:
Respiration is the process whereby oxygen is brought into the cell for use in metabolism. In our bodies, This is involves a transportation process: from atmosphere via airways to the lungs; across membranes to the blood; into red blood cells carried by arteries to tissues, then across membranes again to interstitial fluid and then into cells. Whether your brain functions at altitude depends not only on the amount of oxygen you deliver to your nose or mouth but also on whether your entire respiratory system functions properly.
The Respiratory Scheme:
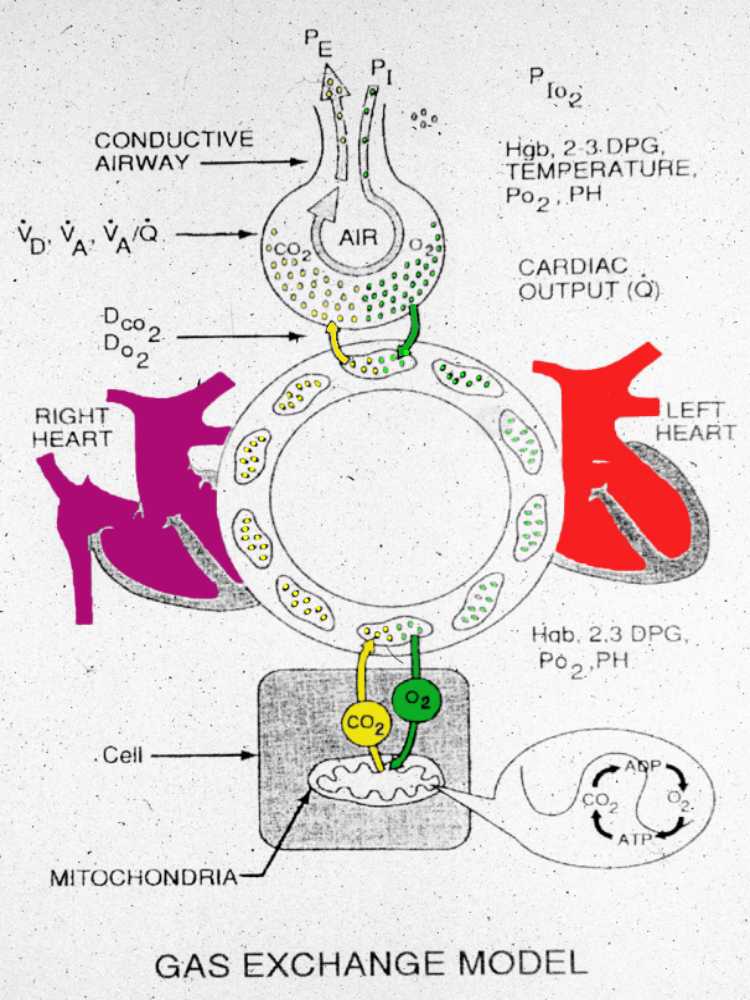
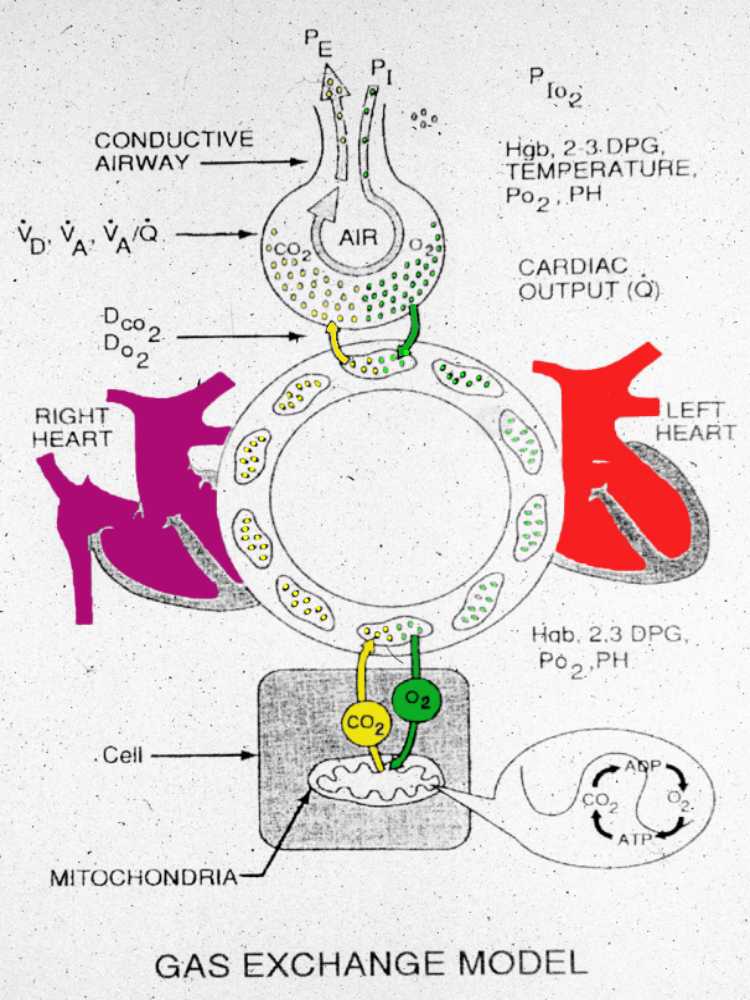
Figure
2: Graphical representation of the respiratory and circulatory
systems.
This is a cartoon of the respiratory and circulatory systems of our bodies. Oxygen is drawn into our lungs, crosses the alveolar membrane into the blood stream where it is carried within the hemoglobin molecule to very distant capillaries. There the oxygen transverses other tissues and eventually enters the cell. Within the cell it finally enters the mitochondria where it is used to oxidize sugars to produce the energy we use. At many points along this system, the process of oxygenation may be interrupted or embarrassed.
Breathing.
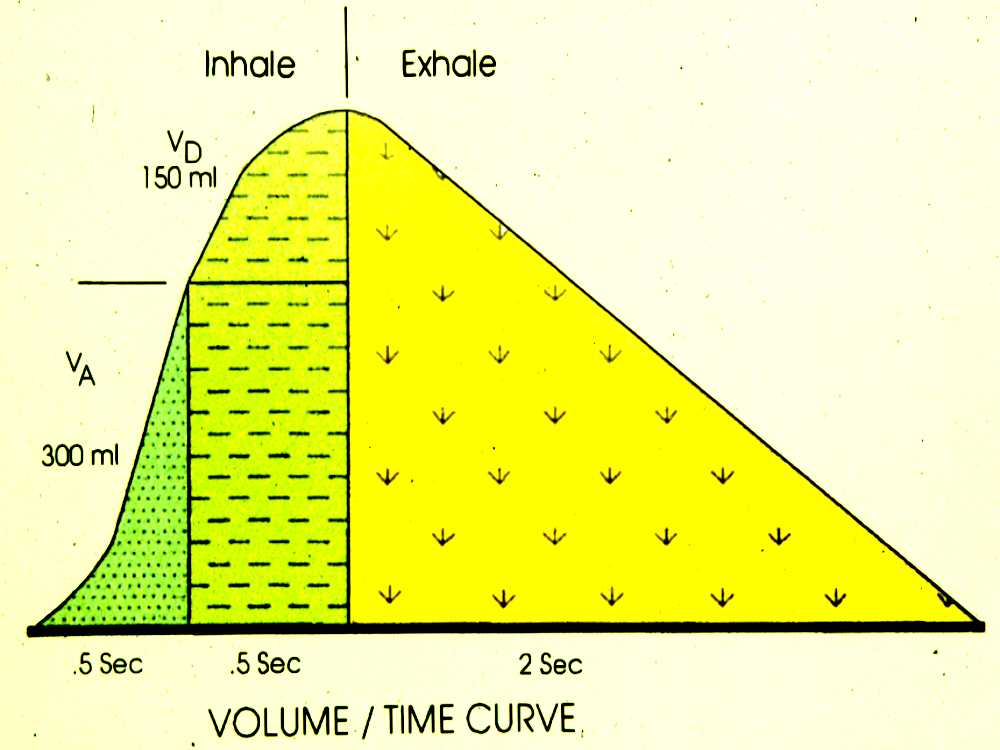
The first stage of respiration involves breathing: Let's look at how we get air -- which hopefully contains oxygen -- into our bodies. Look at Figure 3, and note that there's a fairly large volume of air that simply fills up our airways and isn't involved at all in gas exchange: this is called "dead space." This dead air doesn't "count" in getting oxygen into our bodies, because it contains the same low amount of oxygen as does exhaled air. Each breath must exceed the volume of dead space by enough to bring in the oxygen we need (and to get rid of carbon dioxide).
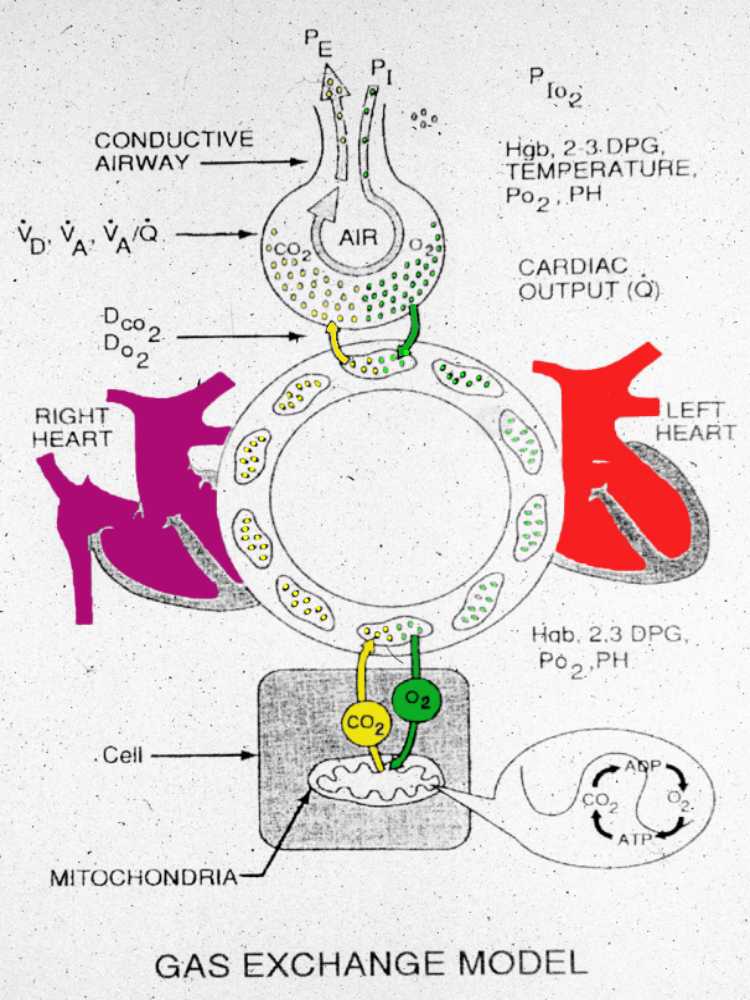
Figure 3 A graph of inhalation and exhalation showing the initial dead space, the first part of each breath. (Same as fig 15.
This three color drawing shows the normal person's breathing pattern. The darker green area on the left represents the first portion of each breath we take. That portion of the breath goes deepest into the lungs, right out to the alveolar walls where the air-blood interchange takes place. This is the part of our breath from which we extract oxygen, and represents only about 1/3 of each breath. The second portion, colored lighter green, represents the volume of air that we breath in that follows and fills the larger airways but does not take part in respiration. The yellow area is the exhaled gases, plotted against time.
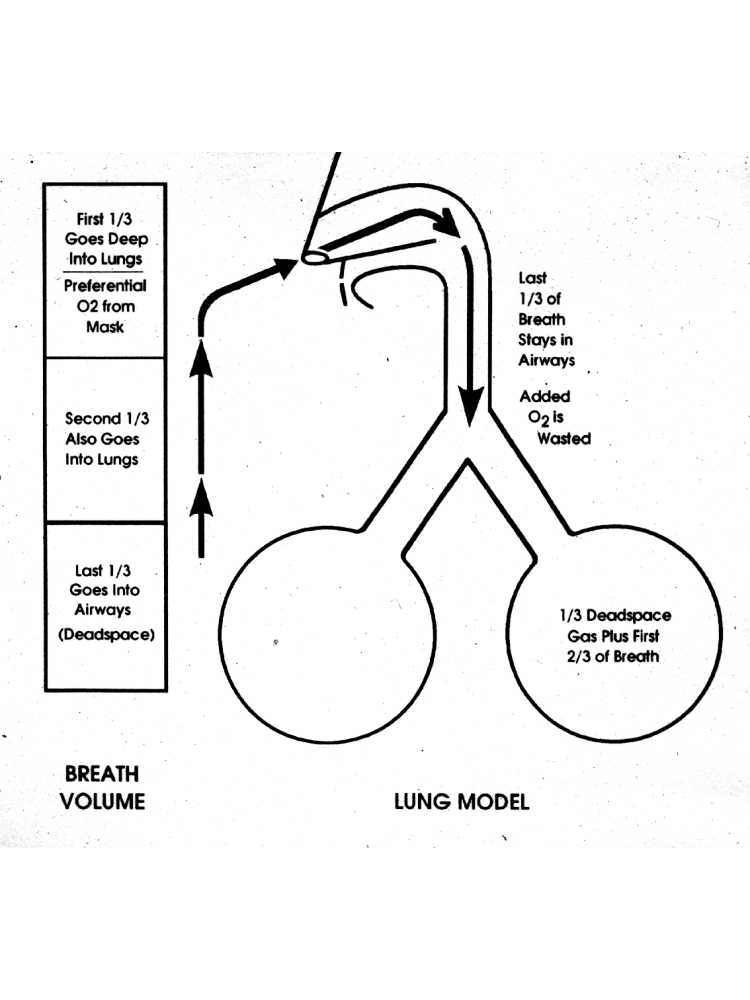
Figure 4 Anatomical representation of the airway and lung showing ventilation and dead space.
The first portion of the breath provides most of our oxygen delivery. As a breath begins, there already is air in the wind pipe and lungs equal to the last 1/3 of the previous breath. During the first third of the breath, this is sucked into the lungs. After inhalation, the air now out in the lungs at the air-blood interface is the residual portion of the last breath, diluted by the first third of the new breath. The last third of each breath only fills airways like the major wind pipes, and no oxygen is extracted from it. Based on this, where would you like to add additional oxygen? Clearly, in the first third of each breath, because it goes the deepest into the lungs and participates in gas exchange.
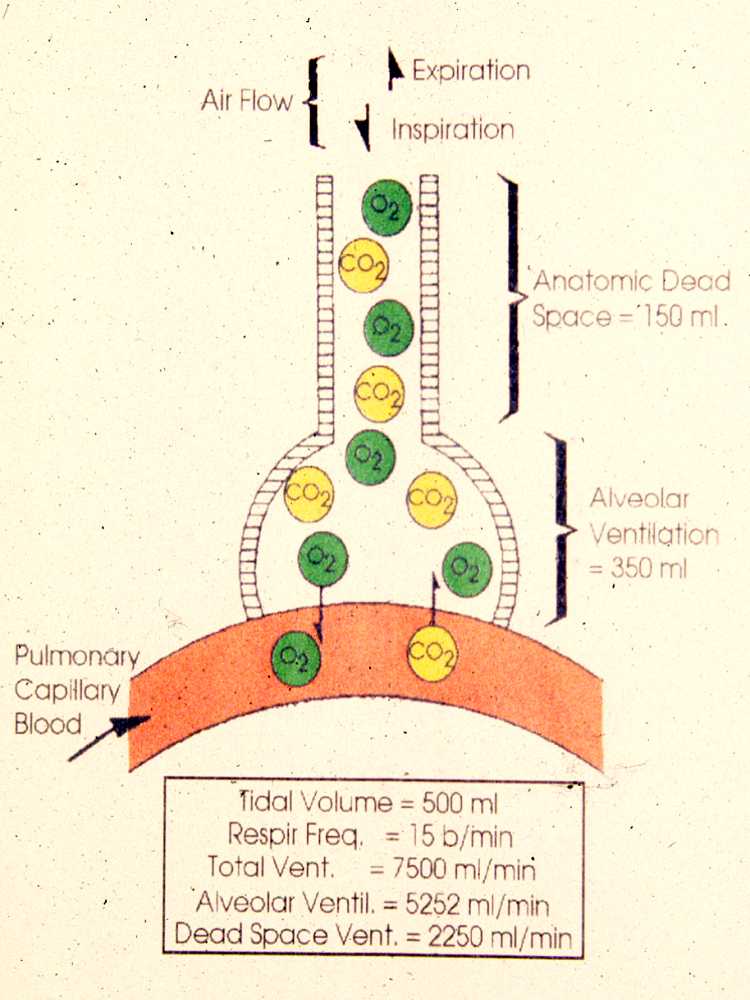
Figure 5 Oxygen enters the body and Carbon Dioxide leaves via the alveolus.
In this figure you see a model of the alveolus, its capillary and gases as represented by green for oxygen molecules and yellow for carbon dioxide. Of all the air that enters the lung only the air adjacent to the alveolar-capillary junction participates in gas exchange.
Figure
6 The ventilation-circulatory interface, normal and certain disease
states.
@begin(comment)
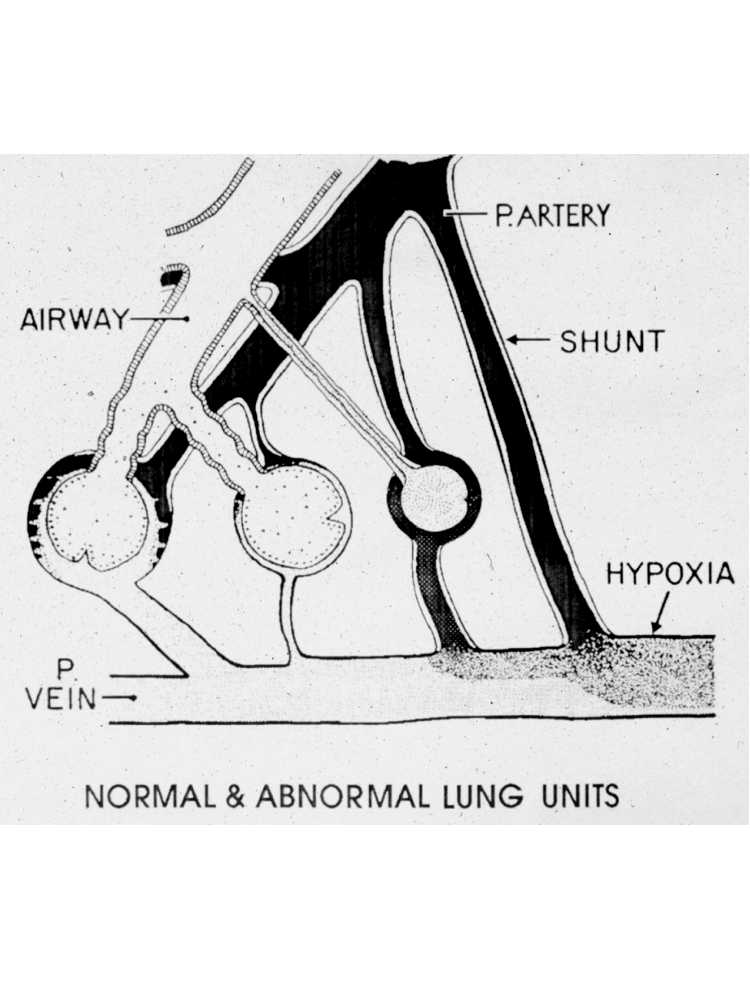
Unfortunately the lung and pulmonary circulation are not perfect. There are differences in the amount of blood and air going to different areas of the lung. These may be physiologic, meaning normal or pathologic, meaning due to disease. As an example, while you are sitting in your seats more blood is doing to the bases of your lungs and more air is going to the tops or apices. This produces a relative mismatch of air and blood. But on the average it works out fine. Shown here are four variations of a constant spectrum. From left to right, are normal, lots of air and very little blood, very little air and finally lots of blood and no air at all where the blood already somewhat depleted of oxygen and darker red essentially bypasses the lung.
Figure
7 Common types of hypoxia.
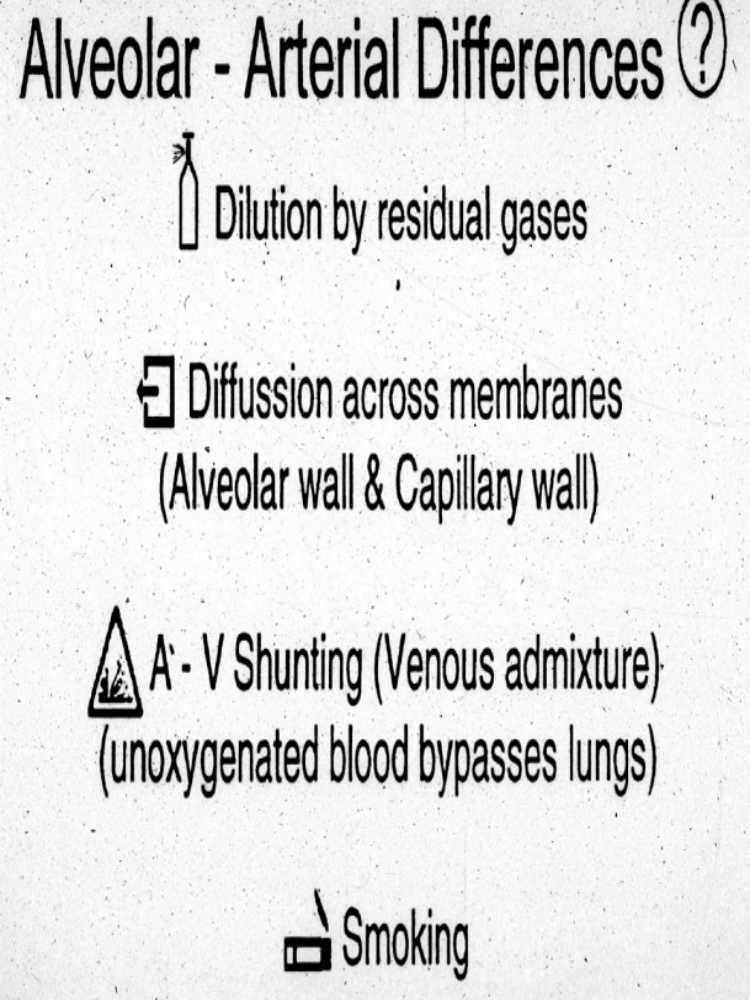
Various disease states including the more common ones of asthma and smoking cause such changes. What has to be considered is that the lung is an inefficient organ at best but is wonderfully efficient in that it keeps us living for many years. In essence it does a job of self regulation providing oxygen to the blood stream to nourish our bodies. Compared to the amount of oxygen in the lungs, the level of oxygen in the blood stream lags the lungs by approximately 10%. Some of the factors causing this are listed on this slide. Remember the residual gas left in the lungs and airway before the next breath, this causes some dilution as well as does humidification (addition of water) and carbon dioxide excretion. For oxygen to get into the bloodstream it has to cross several membranes. That is not particularly easy for an insoluble gas. Certain disease states increase the amount of shunting (bypassing), that is allowing unoxygenated blood to bypass the lung. Lastly, smoking has a tremendous effect upon the normal lung by causing constriction of the airways, destruction of alveolar walls and gas exchange surface and drastically increasing the shunting mentioned before.
Let's now leave physiology and investigate some of the physical world around us.
@end(comment)
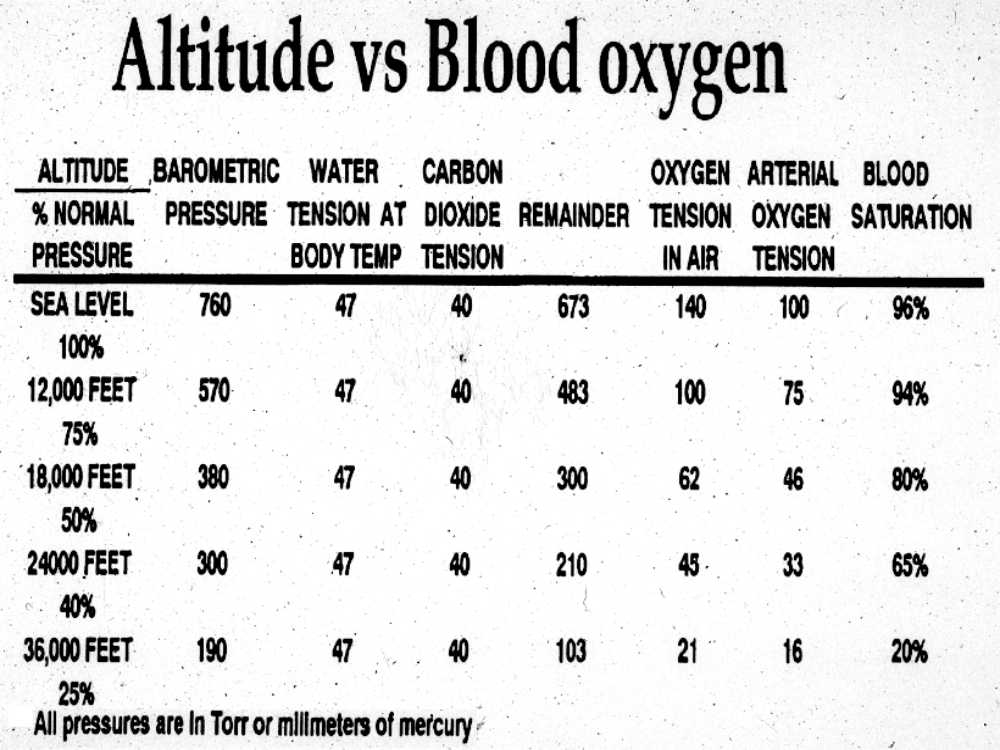
Figure 8 Partial pressures of gases at various altitudes with the corresponding oxygen pressure of the atmosphere and the blood oxygen saturation that would occur in a pilot.
Let's turn our attention to the atmosphere in which we fly. This figure depicts on the left, altitude and the percent of the atmosphere above our heads. For instance at 18,000 feet (5,500m) only 50% of the atmosphere is left, thus we are above 50% of the earth's atmospheric blanket. At 36,000 feet (11,000m) 75% of the atmosphere is below.
The next column represents the atmospheric pressure at each altitude in mm of Hg. We humidify the air we breathe and the vapor pressure of water at body temperature is 47 mm Hg, reducing proportionately the amount of oxygen available. In addition we excrete carbon dioxide as a metabolic waste product. The carbon dioxide level in our blood is virtually constant, regulated by our brains, to 40 mm Hg. The air we breathe in is diluted by humidification (47 mmHg) and by the carbon dioxide excreted into it (40mm Hg).
The oxygen has already been diluted by the residual air from the previous breath. Column 5 shows the pressure after this 87 mm Hg is subtracted from the atmospheric pressure Column 6 shows the oxygen pressure assuming the usual oxygen content of 21%. Column 7 shows the pressure of oxygen after the process of transferring it into the blood stream.
You can see from this table that at altitude, oxygenation can be significantly lower than desired. For example, compared to sea level only one third the amount of blood oxygen should be available at 24,000 feet (7250m).
The last column lists oxygen saturation. This indicates how far the oxygen cells are from being saturated with oxygen at any particular altitude. This is the important number that relates to function: in the low 80's %, you've lost some IQ points and in the 60's% the rest of your cells aren't working so well, either.
Figure
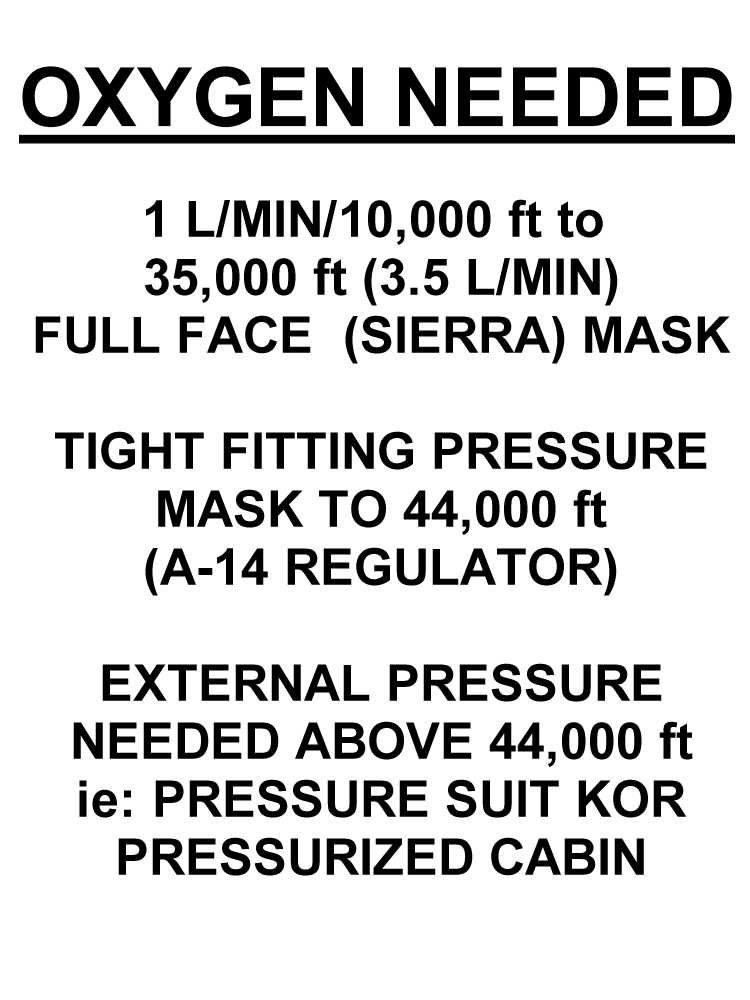
9 Oxygen requirements by altitude.
The aviation community, in the late 1930's and early 1940's, obtained data upon which a guide specifying the rate of supplemental oxygen needed for altitude it is:
1 liter/minute per ten thousand feet: Thus at at 10,000 feet (3,000m) one liter per minute is required; at to 35,000 feet (10,000m) 3.5 liters per minute.
A tight fitting pressure mask is required from 35,000 to 44,000 feet (13,500m)(e.g, an A-14 regulator);
External pressure is needed above 44,000 feet (13,500m): a pressure suit or a pressurized cabin is necessary, because at this altitude the boiling point of blood is below body temperature. This causes a quick death, but not a painless one.
Since very few of us will go above 35,000 feet (10,000m) or yet above 44,000 feet (13,500m) simple systems of oxygen delivery will suffice. There is only one pressurized sailplane known to Dr. Lipe, in the Boeing Museum in Seattle, WA.

Figure 10 A-14 system on, canopy closed. -----------
Various oxygen systems.
Figure
11
Present day oxygen systems fall into five categories:
Mouth tube or nasal prongs
Oxygen conserving canula
Sierra mask and reservoir bag
A-14 regulator and mask (100% and pressure breathing)
Pressure suit or pressurized cabin
Dr. Lipe enlisted Resusci Annie, The famious CPR manikin, to demonstrate oxygen systems.

Figure
12 Mouth tube.
Here you see Annie sitting in the cockpit with a simple tube in her mouth and a ball flow regulator on her chest. This simple system is fairly good at levels below 18,000 (5,500m) feet but should use flows of 1 l/min/10,000 feet (3,000m) up ot 1.8 l/min at the maximum VFR-legal altitude of 18,000 feet (5,500m).

Figure
13 A-14 system.
The other extreme, available to us is an A14 system. A14's are overhauled Air Force surplus. It is a system which will blend oxygen based upon altitude and then begin to increase pressure against exhalation in order to maintain sufficient oxygen pressure in the lungs. It is not automatic.

Figure
14 Oxygen-Conserving Canula.
The conservation canula is the most commonly used oxygen unit for gliders. It is approved by the FAA; it uses oxygen flows of only 30-50% of that required by tube systems up to an altitude of 18,000 feet (5,500m). Its magic is discussed next.
Figure
15 Inhalation-Exhalation volume graph showing Dead Space.
Remember the breath-time diagram (Figure 3). If we want added oxygen to be used most efficiently, we should add it to the very first portion of the breath so that it reaches the furthest into the lungs, into the alveolar air sacks, next to the capillaries. Any added oxygen added in late inhalation or exhalation will not reach the capillaries and will be exhaled and wasted.
@begin(comment)
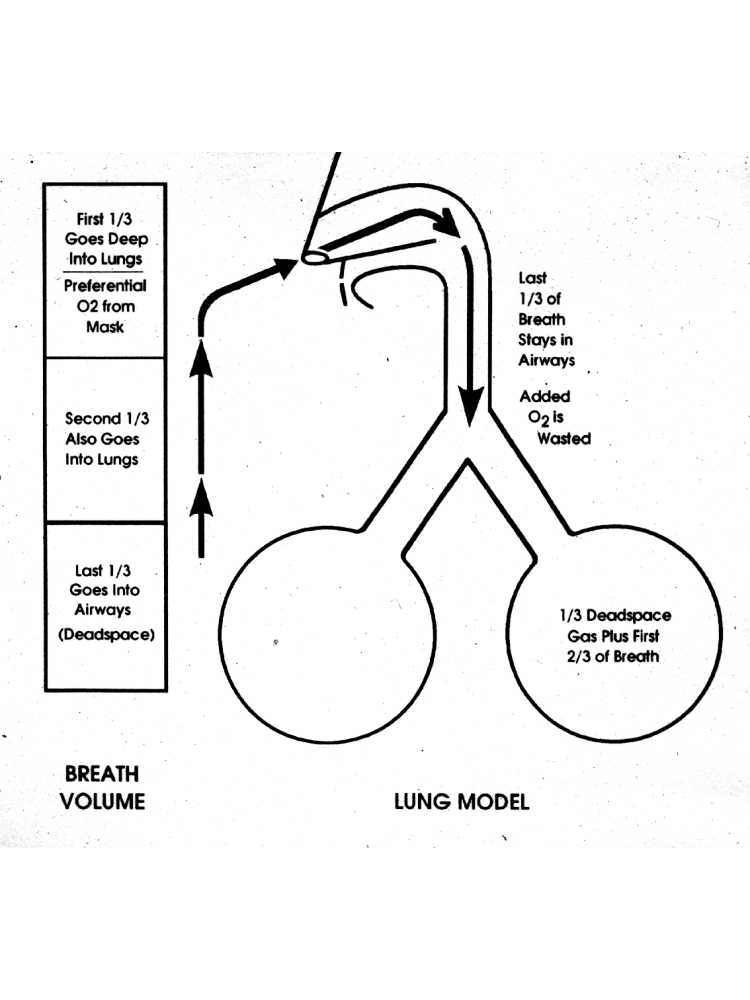
Figure
16 Airway with dead space and wasted ventilation.
Let's reconfirm that idea using the nose-windpipe model also seen earlier. If we add oxygen to the first third of the breath it will go deeper into the lung, whereas any oxygen added to the middle and especially the last thirds will again be wasted.

Figure
17 A hospital oxygen mask.
Here is a mask and bag, it is much cheaper than a Sierra mask system. But don't even think about using it! In the cold of altitude the bag will be so stiff it won't fill because there is no valve on it. The mask fits very poorly and the holes in the sides effectively make this system very inefficient. This mask is designed for hospital use where flows of 10-15 l/min can be given without much thought of cost or availability, its maximum oxygen concentration is near 50% unless flows of 20 l/min or higher are used.
@end(comment)

Figure
18 Hospital canula.
Let's consider the standard canula. This is a cheap item which can be obtained very easily. In order to be effective it needs an oxygen flow of 1 l/min/10,000 (3,000m) feet in order to provide adequate oxygenation up to 18,000 feet. Refer back to the respiratory volume time curve (figure 3). Oxygen given during the later part of inspiration and throughout exhalation is simply wasted.
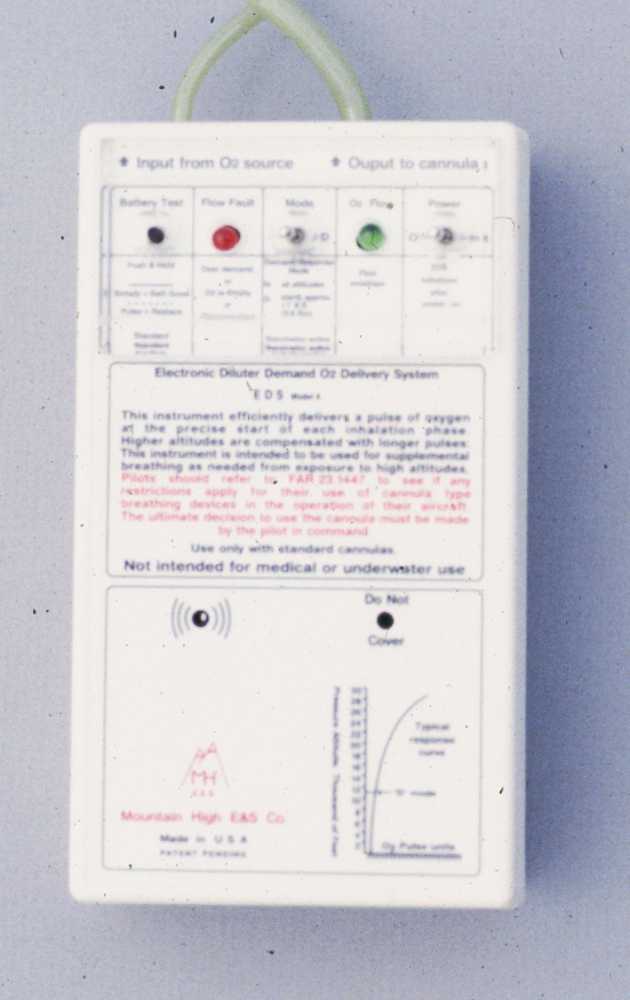
Figure 19 Mountain High's Electronic Delivery System (EDS).
Mountain High of Salt Lake City to the rescue. Patrick Mclaughlin has developed this handy dandy EDS (Electronic Delivery System) oxygen regulator for use with the standard canula. Basically it monitors your breathing by measuring pressure changes at your nostril and when it determines the beginning of inspiration, gives a blast of oxygen, the volume determined by an altitude sensor. It is quite efficient and the little "puff" it emits with each breath reassures you that the system is turned on and working.

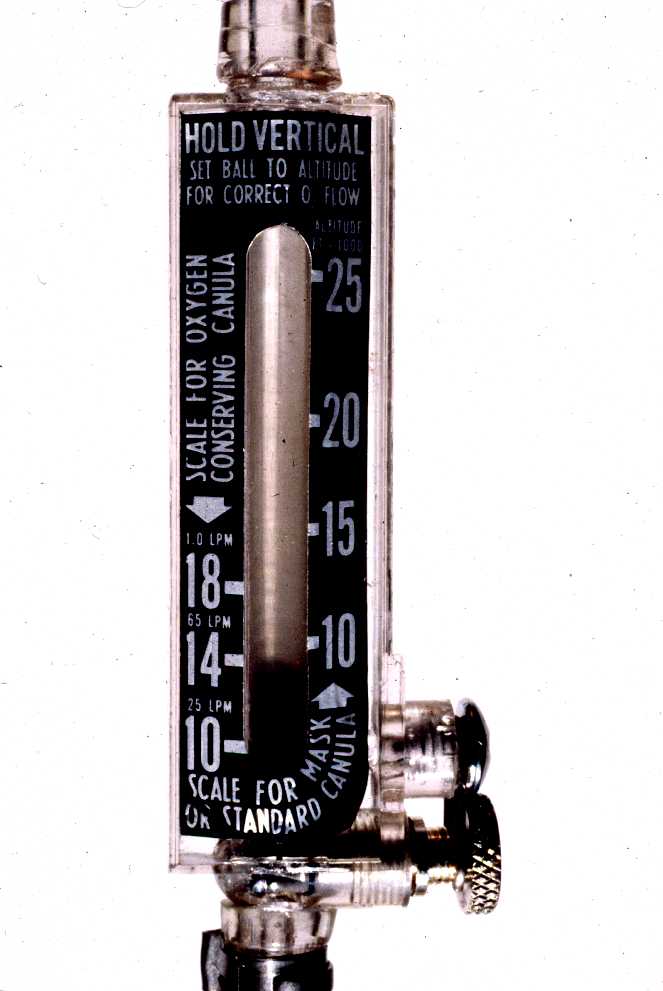
Figure
20 Oxygen-conserving canula and Nelson A-3 flow regulator.
The conserving canula has been quite popular in the Western US. It has two small reservoirs totaling about 15 ml in the cheek pouches that fill during exhalation from a constant flow of oxygen. The nasal prongs are larger than those of the standard canula. This causes most of the oxygen to be delivered during the first portion of the inspiratory (breathing in) phase empties the reservoirs before entraining much ambient air. Thus, compared to the standard canula, its effect has been tested up to 18,000 (5,500m) feet at significantly lower oxygen flows resulting in adequate oxygenation.
The flow meter on Annie's chest produces flows of about 500 ml/min/10,000 feet (3,000m), and is calibrated up to 18,000 feet (5,500m).

Figure
21 Nelson A-3 regulator.
The Nelson A-3 regulator, for use with the oxygen-conserving canula, delivers a constant flow of 600cc/min at 18,000 feet, 1/3 of the flow required if simple non-conserving canula is used.
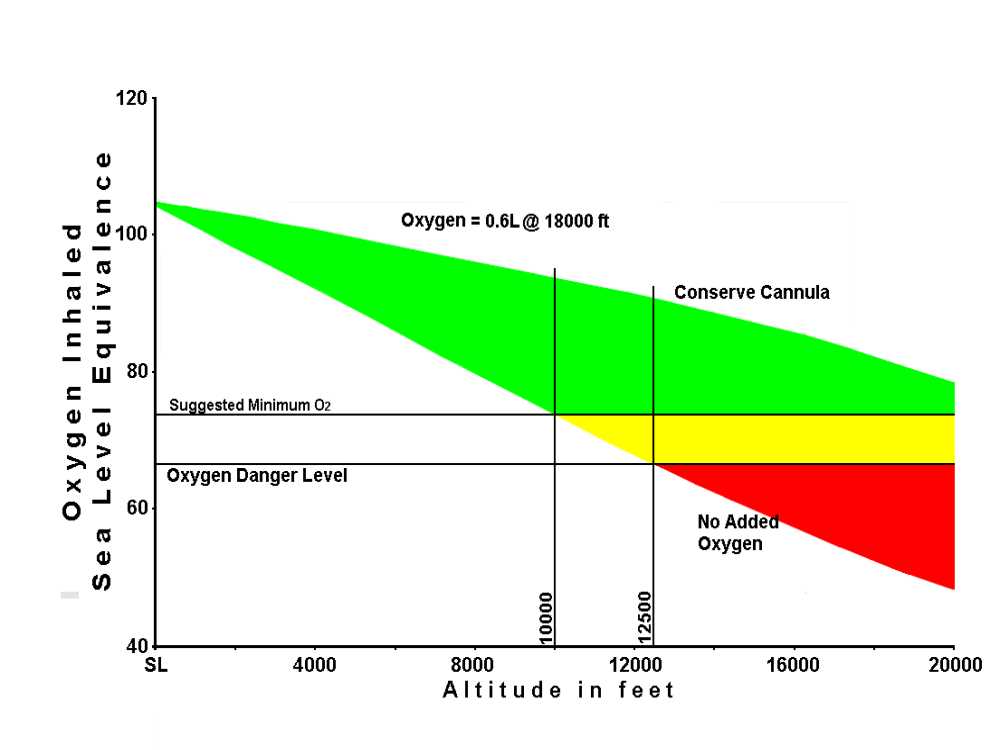
Figure 22 Inhaled oxygen versus altitude, without (lower border) and with oxygen (upper border).
This graph is based upon a mathematical model of our bodies' ability to use the oxygen in the atmosphere at altitude. The lower border of the colored wedge shows the blood oxygen level without supplemental oxygen; the upper border shows the blood oxygen with proper use of an oxygen conserving canula and Nelson (TM) A-3 regulator.
This graph, colored to indicate safe, cautionary, and danger areas, shows that without supplementation your oxygenation would be marginal at 9-10,000 feet (2,700-3,000m) and dangerous above 12,500 feet (3,750m). To use oxygen below the altitudes required by FAA regulation provides a margin of safety to 20,000 feet (6,000m).
[Insert here FAR on oxygen mask use]

Figure
23 Sierra Mask and Nelson A-4 flow regulator.
The next step up in efficiency is the Sierra mask system. This is a tight fitting mask with a head strap and a reservoir bag. Notice the pale rings at the mask-bag juncture. Located there are valves that require the deflation of the bag prior to entrainment (adding in) of outside air. Additionally, exhaled air is prevented from filling the bag and there is slight resistance to venting exhaled air. One note of caution: don't expect the bag to fill visibly. Below 20,000 feet (6,000m) the oxygen flow does not seem to expand the bag. At higher altitudes, 30,000 feet (9,000m) and above, it becomes quite obvious that the bag is filling. This mask system is useful up to the high 30 thousands.
Figure
24 Nelson A-4 flow regulator (1L/mim/10,000 feet).
The Nelson A4 flow regulator has two scales. On your right, 10-25 thousand feet (7,500m), is for use with a sierra mask, calibrated for a flow of 1 l/min/10,000 feet 3,000m), or a standard canula. The left scale is used with the conservation canula. The sierra mask system is at least as efficient as the conservation canula, but is designed to be used above 18,000 feet (5,500m).

Figure 25 Military A-8 oxygen system and Sierra Mask with microphone.
Another frequently used method of regulating the oxygen flow is the A8 regulator. Also an Air Force hand-me-down, these regulators are very susceptible to maladjustment and flow errors. Frequently, these units are red tagged by a maintenance shops, thus becoming paper weights. Their advantage is that they are easily adjustable, with a readout in thousands of feet.
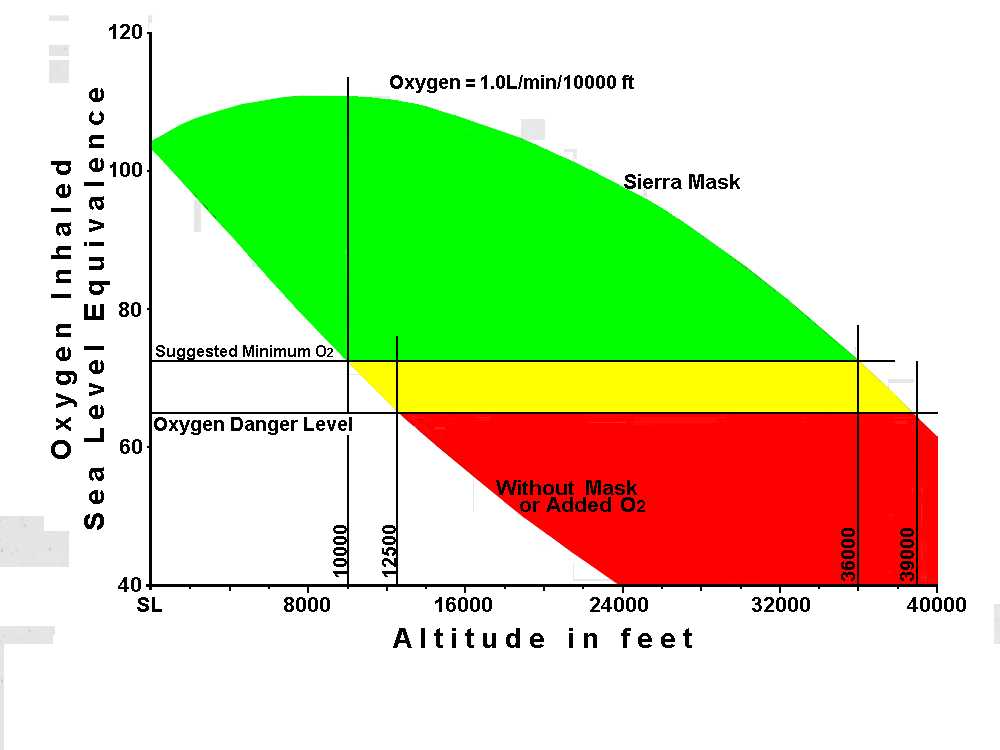
Figure 26 Sierra Mask System versus no oxygen to 40,000 feet.
This is like Figure 22, but taken to a more extreme altitude, in order to show the reserve provided by a full fitting face mask with aconstant-flow reservoir bag (Sierra Mask system) and a delivery rate of 1.0L/min/10,000 feet.
Note that the no-oxygen curve enters the mortuary at about 24,000 feet. The Sierra mask when used correctly, enters the caution range about 36,000 feet (11,000m) and the danger area at about 39,000 feet (12,000m). Dr. Lipe has personally used this system over 37,000 feet (11,500m).

Figure 27 The Altox system.
This interesting system is called the Altox system. It uses a pressurized supply between 20 and 60 pounds per square inch. The black body attached to the nose of the mask is a regulator which is sensitive to mask pressures produced by breathing. It is not very efficient in that it requires constant oxygen except for a small blend hole on the side by the silver lever. Dr. Lipe is interested in paperwork and documentation on this unit. If any one has documentation, please send copies to Dr. Lipe.

Figure
28 Dr. Lipe's own oxygen system.
This is the venerable A14 system. These are surplus military units. On the face is a dial to change the oxygen concentration and back pressure so that it can be used to 44-45,000 feet (13,500). Above 39,000 feet (12,000m) the unit produces resistance to exhalation so that in the low 40 thousands it is somewhat difficult to breathe. It is like trying to breathe with an air compressor in one's mouth.

Figure
29 Military A-14 system.
This Glaser-Dirks has been equipped with a dual oxygen system. There are two bottles, each with its primary regulator adjusted so that they will work in a cascade system. In addition, there are secondary regulators for constant flow systems, regulators for higher pressure systems such as the Altox and EDS from mountain high and an A14 system. Essentially each system can work off either tank automatically. This was Dr. Lipe's fun ship and test bed.
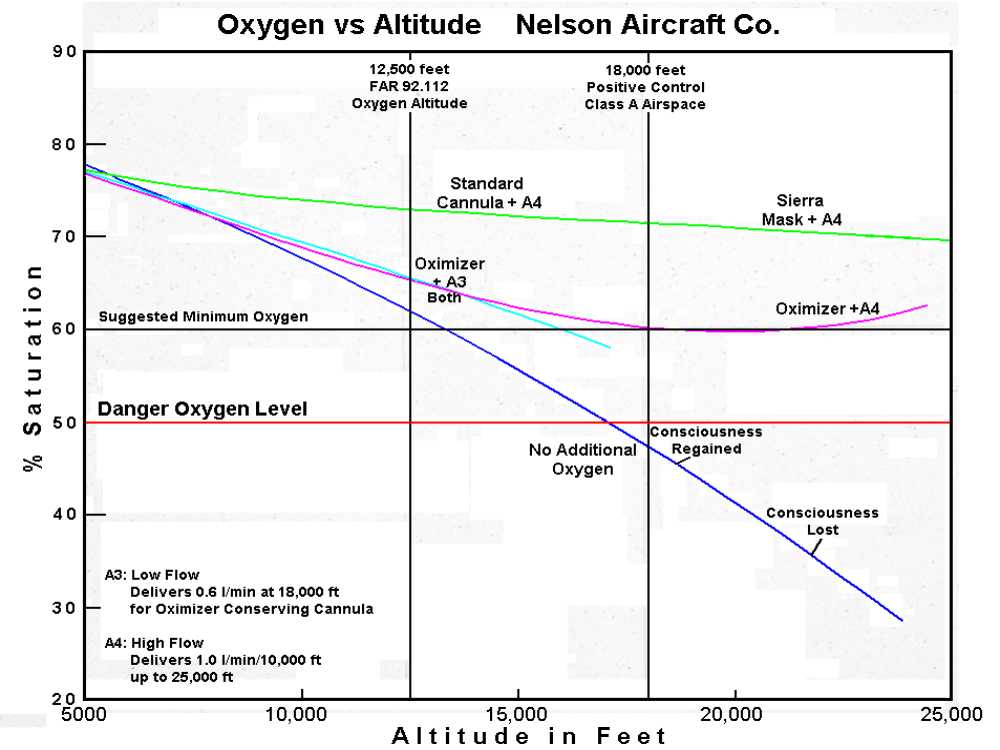
Figure 30 Performance of the Nelson flow systems during developmental testing.
Several years ago during the development of the Nelson A3 low flow regulator, Dr. Lipe accompanied Ted Nelson and his son Jerry and a pilot on a data gathering flight to 24,000 feet (7,250m). Several systems were evaluated as are shown in this chart. The measurements were accomplished by an oximeter, a device which uses photocells to measure the color of the capillary blood by spectral absorption at 600 and 630 milli-microns. Altitude was called out by the pilot. Ted Nelson was the recorder and Jerry was the guardian. Dr. Lipe was the guinea pig.
The first climb to 24,000 feet (7,250m) was done as a control, without added oxygen. This resulted in Dr. Lipe losing consciousness. Previously he had been to 24,000 (7,250m) feet, without added oxygen, in altitude chambers, without adverse effect. The last event Dr. Lipe remembers was 22,000 feet (6,750m). After reaching 24,000 feet (7,250m) the pilot started down and Dr. Lipe woke up at about 19,000 feet (5,750m). According to Jerry Nelson, Dr. Lipe still acted normally, although his speech was a little slurred. The middle curve was accomplished using a conserve canula and an early A3 flow regulator to 18,000 (5,500m), switching to an A4 regulator above that. The top curve was a standard canula using an A4 regulator to 18,000 (5,500m) and then a Sierra mask above that. Obviously the top curve is best. It was felt that the middle curve was marginal. Based on this data, the A3 flow regulator was modified to increase delivery volume at higher altitudes by about 25% before it was put on the market.
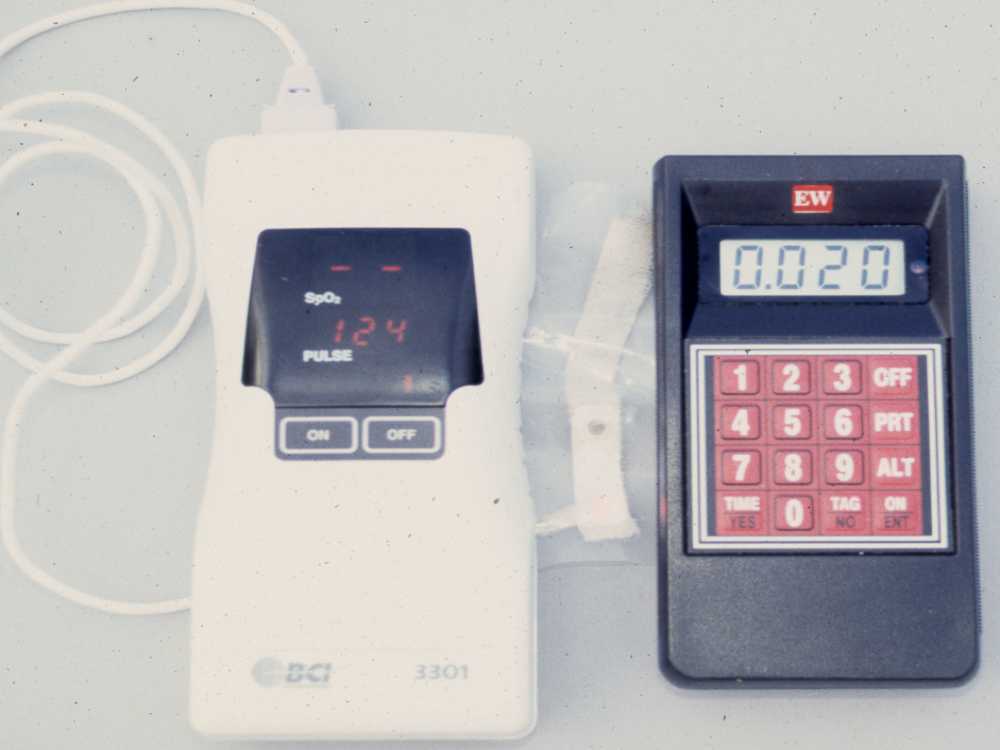
Figure
31 Portable oximeter (left) and recording barometer used in studies.
Today the measurement of oxygen saturation and altitude is easy. This little oximeter on the left -- a DCI 3301 -- can be put in a pocket and the barograph on the right is of similar size. Each will record data. The data only needs to be downloaded and synchronized.
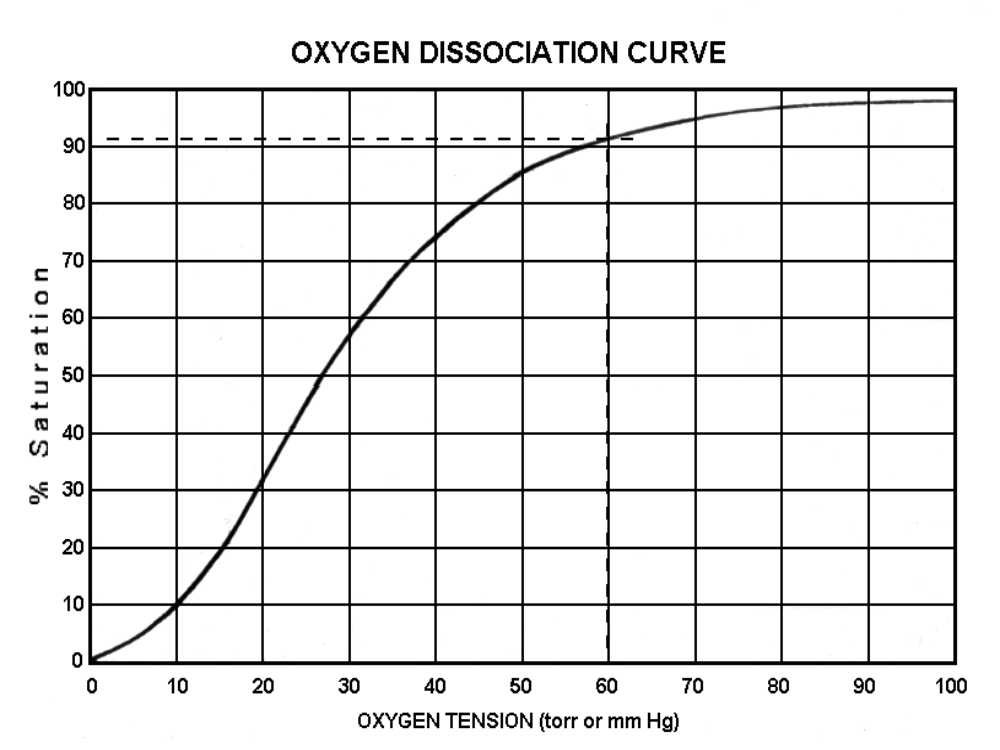
Figure 32
Oxygen saturation is not linearly related to oxygen tension. This is because the hemoglobin molecule has a changing affinity for oxygen. The equipment Dr. Lipe uses to measure oxygen in flight measures saturation. This needs to be converted into oxygen tension for our use. Essentially, the steepness of this curve corresponds to hemoglobin's ability to release oxygen. For instance, between the oxygen tensions of 20 and 30 more oxygen is released than between 60 and 70. Incidentally, at sea level, the use of 100% oxygen only increases blood carried oxygen by three tenths of one percent. At altitude when our saturation is lower extra oxygen is very beneficial.
@begin(comment)
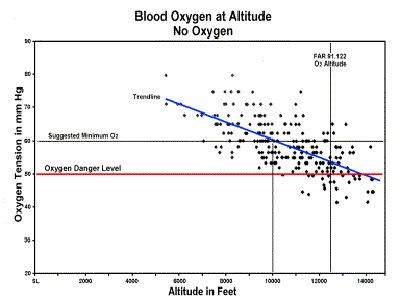
Figure
33 (LipeRevisedFigures32)
Here Dr. Lipe has plotted several flights below 18,000 feet (5,500m) using the ordinate for blood oxygen tension and the abscissa for altitude. A calculated trend analysis line is shown in blue. Note the relationship of the trend line to altitude.
This shows a flight without supplemental oxygen. The scatter of the data points demonstrates the variability of the measurement system used; the blue line is a line of best fit, showing that the data have the expected relationship between oxygen saturation and altitude.
It crosses the danger level, that level where thought and decision processes begin to be compromised, about 12,500 feet (3,000m). Also the line crosses what Dr. Lipe consider to be the top of the yellow caution area about 10,000 feet (3,000m). This data is in support of the mathematical model without oxygen.
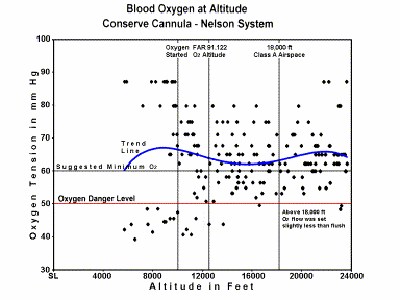
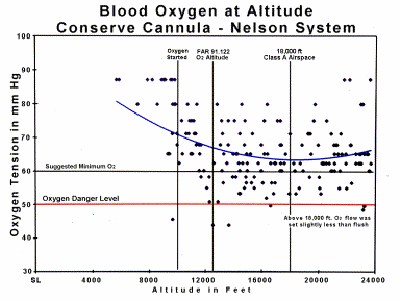
Figure 34
(LipeRevisedFigures33
This figure represents a 4 hour flight from Truckee into wave south of Minden and was purposely limited to 24,000 feet. It was a series of 4 climbs during that time from 14,000 to 24,000 then back down to 14,000 and then over again 3 more times. At the end of the flight Dr. Lipe went back to Truckee and passing through 12,500 feet removed my nasal canula. The figure shows the data points and a third-order curve of best fit. Dr. Lipe was very curious why there were data points below 12,500 and below 50 mm torr oxygen tension. He thought that they were bad data, but in reviewing the data carefully, he discovered that most of the bad points were at the end of the flight, during the final phase of the descent.
He used a nasal canula and a Nelson A3 flow regulator. The trend line shows a bimodal curve which distressed Dr. Lipe when he first saw it. There were three separate climbs from 10,000 feet to 24,000 feet 3,000-7,600m) before returning to Truckee. The A3 flow regulator was set according to the altitude except above 18,000 feet (5,500m) when it was set to just less than flush. Notice that the system behaves very similarly to the mathematical model for the conserve canula showing it effective to the middle 20 thousand foot (6,000m) level. A little investigation revealed that all 16 points in the lower left group occurred during the last 16 minutes of the flight. You will also notice that they are all below 12,500 feet (3,750m) in altitude. Dr. Lipe had removed the oxygen system passing through 12,500 feet (3,750m) while returning to home base.
Either his blood unexpedtedly desaturated at low altitudes where it should not have, or the measuring system became incorrect at the end of the flight. This could have occurred because of displacement of the oximeter's sensor or because Dr. Lipe's hands became cold, decreasing blood flow under the sensor.
Figure
35
LipeRevisedFigures34
This is the same plot as Fig 33, but with the last 7 1/2 minutes of data (the time below 12,500 feet after removal of oxygen, to the termination of the landing and rollout, removed. Now the line of best fit looks as expected.
Why were the aberrant points as they were? Why were all the points after removing the oxygen canula so depressed? If you refer to figure 33, Dr. Lipe should have been in the range of 54 to 70 torr oxygen, not the 40-50 torr range, at these altitudes.
If this were purely due to measurement scatter, at least SOME of them should be above 50 torr!
When these points are removed the new trend line is now of a much different character. It starts high at lower altitudes and curves down to around 16,000- 24,000 feet (4,900-7,600m) as would be expected.
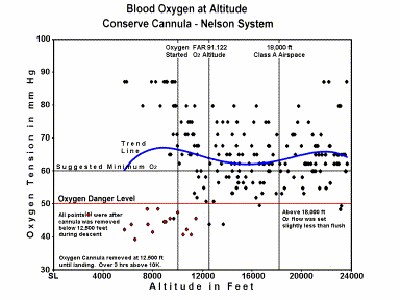
Figure 36 Same as fig 34, but the points off oxygen below 12,500 are red tagged.
LipeRevisedFigures35
In Figures 33 - 36 The fairly wide scatter of points is primarily measurement error due to probe movement, skin temperature fluctuations and so on
In this slide the offending last 16 points, all below 12,500 (3,750m) are marked. These points represent all data during the final 16 minutes of the flight, the altitude was less than 12,500, feet (3,750m) during which time Dr. Lipe was entering the traffic pattern and making his approach to landing. Dr. Lipe does not remember feeling different, although usually quite aware of his own hypoxic symptoms. The real question arises, had Dr. Lipe known of his relative hypoxia would he have remained on oxygen? The answer is a definite YES!
But why are all these data, without exception, aberrant, when for all rightful purposes they should not have been? There is no known physiologic mechanism by which this could occur. This "experiment" has never been repeated. If you believe this data represents a real phenomenon, the only proper action is to do what was advocated many years ago: Once using oxygen, continue it until roll out stops.
@end(comment)
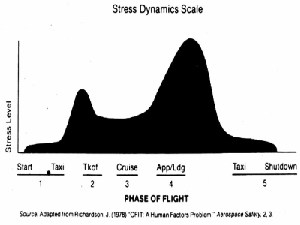
Figure
37 Stress versus flight stage
The stress of piloting on a time line. Don't forget you are tired, probably dehydrated, entering the airport traffic area and proceeding to a landing, all actions together, probably, the most dangerous part of the flight and hypoxic as well. At this time our thought processes and judgment patterns need to be the sharpest since we took off.
Now a thought that philosophers have pondered for years. If nobody is around to hear a meteor crash in the forest, does it really make noise? To put that in glider terms; does it really hurt when you hit the ground while you are asleep?
Last,
Experience is a wonderful thing
It allows you to recognize a mistake
When you make it again
slipe@earthlink.net